A State of Denial: How to Lessen the Impact of Denials on Collections and Speed Up the Process
As the number of payer denials continues to increase, it is crucial for physician practices and ASCs to stay informed about increasingly complex payer requirements, especially concerning coding, prior authorization, timely filing, and appeals processes. However, keeping up with these requirements can be a demanding task, often requiring dedicated staff members – a luxury in today’s healthcare environment – to oversee and spend countless hours pursuing resolution.
Research shows that more than ten percent of all claims were denied in 2022, an increase of close to eight percent from 2021.
Categorizing Denials
To tackle denials effectively, the first step is categorizing them in your practice management system. This categorization will allow you to identify problem areas. Common categories of denials include:
Registration: Errors in patient information and demographics.
Eligibility: Issues with patient insurance coverage.
Credentialing: Problems related to provider qualifications.
Authorization: Lack of proper authorization for services.
Coding: Mistakes in medical coding.
Bundling: Errors in bundling multiple services into a single claim.
Timely Filing: Claims not submitted within the required timeframe.
Categorizing denials helps you pinpoint where mistakes are occurring and conduct a root cause analysis, providing real-time visibility into trends and issues that contribute to denials. Understanding the underlying causes of denials is crucial to preventing them in the first place. For instance, it might become evident that the front desk staff doesn’t understand the difference between Medicare and Medicare Advantage plans, or that physicians are struggling with new coding rules. Categorization helps focus your efforts on the areas that need the most attention.
Preventing Denials with Rules Engine Technology
When it comes to denial prevention, the importance of rules engine technology cannot be overstated. Every healthcare practice should employ this technology to ensure claims are error-free before they are submitted. Rules engine technology is very effective when designed to:
- Identify and Re-Route Claims with Errors
- Auto-fix Claims Before Submission
This streamlines the claims submission process, minimizing the chance of denials. At Koha Health, we’ve seen great results with this powerful tool.
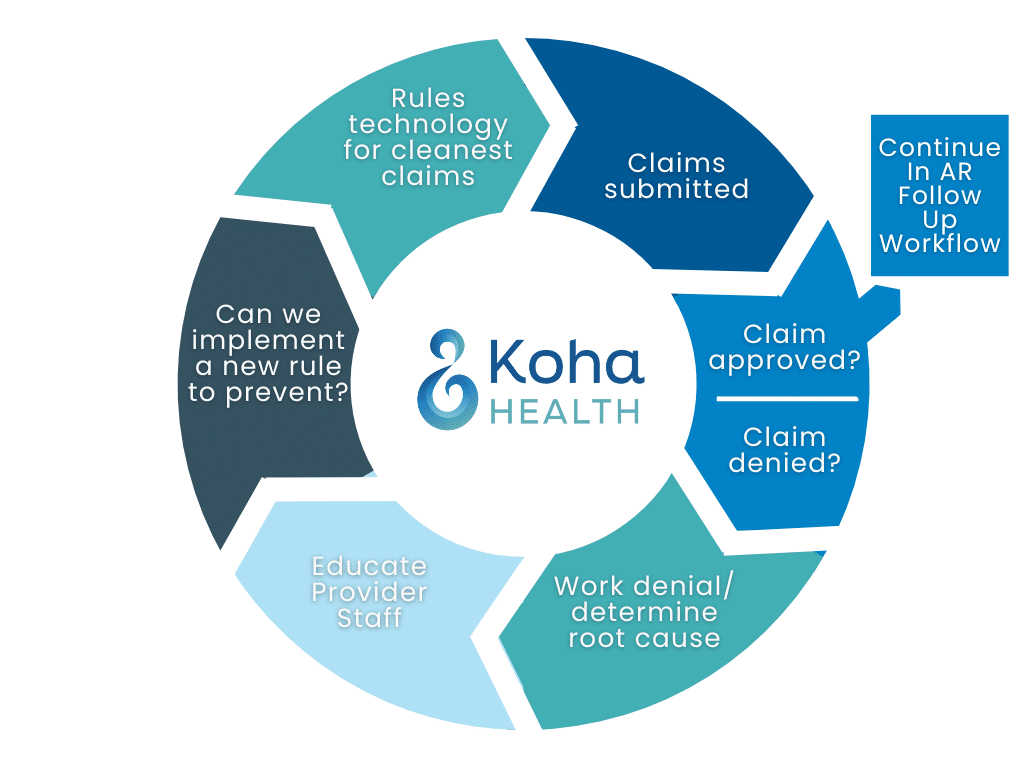
A Better Denial Workflow
When denials do occur, it’s crucial to rely on tech-enabled solutions coupled with expert coders to realize efficiencies. New technology solutions streamline and improve the denial workflow in several ways. New technology helps streamline, categorize and group like denials, then flags them for staff to prioritize, increasing efficiency.
Combining rules engines with artificial intelligence creates a seamless process requiring human intervention only on complex issues.
With complex denials being served to staff as needed, it allows them to be more productive and work through the denials queue systematically (ensuring they are worked in order and not passed over in favor of an easier case). This approach minimizes backlog and accelerates revenue recovery.
The reporting generated in a tech enabled denial workflow feeds back into the root cause analysis process, enabling you to identify the education needed and new rules to be created. Altogether, this creates a continuous improvement cycle, making your denial management system more robust and efficient.
Conclusion
Denials may be a constant issue in physician practices and ASCs, but with the right approach, they can be managed effectively. Categorizing denials, preventing them with rules engine technology, and streamlining and improving the workflow with new technology are all critical components of a successful denial management strategy.
Koha Health offers seamless, interconnected, best-practice revenue cycle workflows from patient registration to final adjudication, generating accurate and timely reimbursements, reduced operating costs, and an overall better patient experience.
Designed to leverage existing investments in technology and people, Koha Health offers a strategic support system driving meaningful improvement that flows to the bottom-line.